What is Periodontal (Gum) Disease?
The term “periodontal”means “around the tooth.” Periodontal disease (also known as eriodontitis and gum disease) is a common inflammatory condition which affects the supporting and surrounding soft tissues of the tooth; also the jawbone itself when in its most advanced stages.
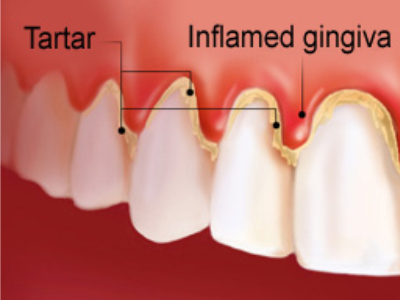
Periodontal disease is most often preceded by gingivitis which is a bacterial infection of the gum tissue. A bacterial infection affects the gums when the toxins contained in plaque begin to irritate and inflame the gum tissues. Once this bacterial infection colonizes in the gum pockets between the teeth, it becomes much more difficult to remove and treat. Periodontal disease is a progressive condition that eventually leads to the destruction of the connective tissue and jawbone. If left untreated, it can lead to shifting teeth, loose teeth and eventually tooth loss.
Periodontal disease is the leading cause of tooth loss among adults in the developed world and should always be promptly treated.
Common Causes of Gum / Periodontal Diseases
There are genetic and environmental factors involved in the onset of gum disease, and in many cases the risk of developing periodontitis can be significantly lowered by taking preventative measures.
Here are some of the most common causes of gum disease:
 |
 |
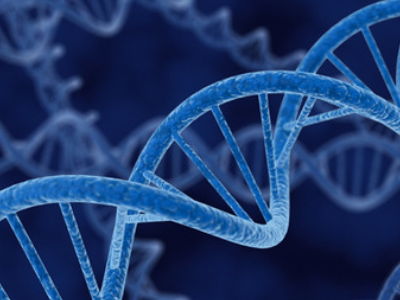 |
| Poor dental hygiene – Preventing dental disease starts at home with good oral hygiene and a balanced diet. Prevention also includes regular dental visits which include exams, cleanings, and x-rays. A combination of excellent home care and professional dental care will ensure and preserve the natural dentition and supporting bony structures. When bacteria and calculus (tartar) are not removed, the gums and bone around the teeth become affected by bacteria toxins and can cause gingivitis or periodontitis, which can lead to tooth loss. | Tobacco use – Research has indicated that smoking and tobacco use is one of the most significant factors in the development and progression of gum disease. In addition to smokers experiencing a slower recovery and healing rate, smokers are far more likely to suffer from calculus (tartar) build up on teeth, deep pockets in the gingival tissue and significant bone loss. | Genetic predisposition – Despite practicing rigorous oral hygiene routines, as much as 30% of the population may have a strong genetic predisposition to gum disease. These individuals are six times more likely to develop periodontal disease than individuals with no genetic predisposition. Genetic tests can be used to determine susceptibility and early intervention can be performed to keep the oral cavity healthy. |
 |
 |
 |
| Pregnancy and menopause – During pregnancy, regular brushing and flossing is critical. Hormonal changes experienced by the body can cause the gum tissue to become more sensitive, rendering them more susceptible to gum disease. | Chronic stress and poor diet – Stress lowers the ability of the immune system to fight off disease, which means bacterial infections may possibly beat the body’s defense system. Poor diet or malnutrition can also lower the body’s ability to fight periodontal infections, as well as negatively affecting the health of the gums. | Diabetes and underlying medical issues – Many medical conditions can intensify or accelerate the onset and progression of gum disease including respiratory disease, heart disease, arthritis and osteoporosis. Diabetes hinders the body’s ability to utilize insulin which makes the bacterial infection in the gums more difficult to control and cure. |
 |
 |
|
| Grinding teeth – The clenching or grinding of the teeth can significantly damage the supporting tissue surrounding the teeth. Grinding one’s teeth is usually associated with a “bad bite” or the misalignment of the teeth. When an individual is suffering from gum disease, the additional destruction of gingival tissue due to grinding can accelerate the progression of the disease. | Medication – Many drugs including oral contraceptive pills, heart medicines, anti-depressants and steroids affect the overall condition of teeth and gums; making them more susceptible to gum disease. Steroid use promotes gingival overgrowth, which makes swelling more commonplace and allows bacteria to colonize more readily in the gum tissue. |
Signs & Symptoms of Periodontal Disease
It is extremely important to note that periodontal disease can progress without any signs or symptoms such as pain. This is why regular dental checkups are exceptionally important. Described below are some of the most common signs and symptoms of periodontitis.
If you have any of these signs or symptoms, the advice of a general dentist or periodontist should be sought as soon as possible:
 |
 |
 |
| Unexplained bleeding – Bleeding when brushing, flossing or eating food is one of the most common symptoms of a periodontal infection. The toxins in plaque cause a bacterial infection which makes the tissues prone to bleeding. | Pain, redness or swelling – A periodontal infection may be present if the gums are swollen, red or painful for no apparent reason. It is essential to halt the progression of the infection before the gum tissue and jaw bone have been affected. It is also critical to treat the infection before it is carried into the bloodstream to other areas of the body. | Longer-looking teeth – Periodontal disease can lead to gum recession. The toxins produced by bacteria can destroy the supporting tissue and bones, thus making the teeth look longer and the smile appear more “toothy.” |
 |
 |
 |
| Bad breath/halitosis – Although breath odor can originate from back of the tongue, the lungs and stomach, from the food we consume, or from tobacco use, bad breath may be caused by old food particles which sit between the teeth and underneath the gumline. The deeper gum pockets are able to house more debris and bacteria, causing a foul odor. | Loose teeth/change in bite pattern – A sign of rapidly progressing periodontitis is the loosening or shifting of the teeth in the affected area. As the bone tissue gets destroyed, teeth that were once firmly attached to the jawbone become loose or may shift in position. | Pus – Pus oozing from between the teeth is a definitive sign that a periodontal infection is in progress. The pus is a result of the body trying to fight the bacterial infection. |
Treatment of Gum Disease
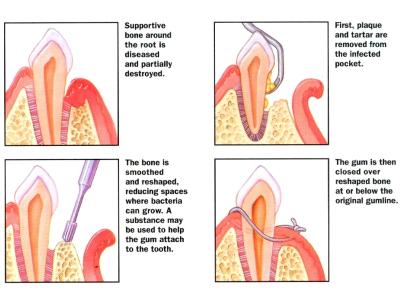
Periodontists specialize in the treatment of gum disease. A periodontist can perform effective cleaning procedures in deep pockets such as scaling and root planing, and also prescribe antibiotic and antifungal medications to treat infection and halt the progression of the disease.
In the case of tooth loss, the periodontist is able to perform tissue grafts to promote natural tissue regeneration, and insert dental implants if a tooth or several teeth are missing. Where gum recession causes a “toothy” looking smile, the periodontist can recontour the gingival tissue to create an even and aesthetically pleasing appearance.
Preventing periodontal disease is critical in preserving the natural dentition. Addressing the causes of gum disease and discussing them with your dentist will help prevent the onset, progression, and recurrence of periodontal disease.
If you have any questions or concerns about the causes or treatments pertaining to gum disease, please ask your dentist.
Treatment for Periodontal Disease
There are many surgical and nonsurgical treatments the periodontist may choose to perform, depending upon the exact condition of the teeth, gums and jawbone. A complete periodontal exam of the mouth will be done before any treatment is performed or recommended.
Here are some of the more common treatments for periodontal disease:
Bone Grafting
Reasons for bone graftsBone grafting is a highly successful procedure in most cases. It is also a preferable alternative to having missing teeth, diseased teeth, or tooth deformities. Bone grafting can increase the height or width of the jawbone and fill in voids and defects in the bone |
 |
 |
There are essentially two basic ways in which bone grafting can positively impact the health and stability of the teeth:
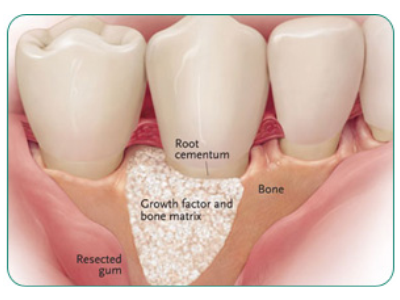
Jaw Stabilization – Bone grafting stabilizes and helps restore the jaw foundation for restorative or implant surgery. Deformities can also be corrected and the restructuring of the bone can provide added support.
Preservation – Bone grafting can be used to limit or prevent bone recession following a tooth extraction, periodontal disease, or other invasive processes.
Oral Examination
Initially, the dentist will thoroughly examine the affected area in order to assess the general condition of the teeth and gums. If periodontal disease is present or the adjacent teeth are in poor condition, these factors will be fully addressed before the bone grafting procedure can begin. The dentist will also recommend panoramic x-rays in order to assess the precise depth and width of the existing bone. On occasion, a CAT scan may be recommended to determine the bone condition. Depending on these results, the dentist may also anesthetize the area and explore into the gum in order to determine what kind and how much bone is required.
What Does Bone Grafting Involve?
There are several types of bone grafts. Your dentist will determine the best type for your particular condition.
The bone grafting procedure can often take several months to complete. Bone is typically harvested from your own body (or on rare occasions obtained from a “bone bank”) and added to the affected site. This bone will fuse with the existing bone and the migration of cells will cause firm adhesion and cell growth. Supplementing the jaw with bone will result in greater bone mass to help support and anchor the implant(s).
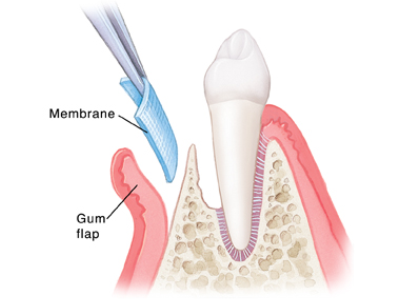
During the surgery, the dentist will numb the grafting and extraction sites using local anesthetic. A small incision will be made to prepare the site for the new bone and it will be anchored into place. On occasion, a synthetic membrane may be used to cover the new bone. This membrane prevents soft tissue and bacterial invasions, and encourages new bone growth. The surgery does not require an overnight stay, and you will be provided with comprehensive instructions for your post-operative care. The dentist will prescribe medications to help manage infection, discomfort and swelling.
Periodontal Splints
Splinting is a technique used to stabilize teeth which have become loose as a result of losing the supporting bone around them to periodontal disease, a condition known as secondary occlusal trauma. Frequently the problem is complicated by heavy bite stress.
 |
There are two basic types of periodontal splinting, with some variation. The first is “extra-coronal splinting”, in which a stabilizing wire, fiber-reinforced ribbon, or similar stabilization device, is bonded to the outsides of the teeth like a fixed orthodontic retainer. The second is “intra-coronal splinting”, in which a slot is milled into the affected teeth, and the stabilizing device is inserted into the slot and bonded in place. This can make the splint less visible, but accomplishes the same goal of immobilizing the teeth.
If the teeth have lost more than 40% of the supporting “alveolar” bone around them, a diagnosis of “severe” periodontal disease is made. Most often, teeth that are mobile (loose) enough to require splinting have that diagnosis. However, if the tooth roots are abnormally short or thin, or if the bone around them is not particularly dense, the teeth may be loose when less than 40% of the volume has been lost. |
| Your dentist can tell you if your teeth are mobile enough to require splinting. Another factor that comes into play is the status of the periodontal disease. If you have active disease, and the bone around the teeth is softened from inflammation, simply bringing the disease under control through other types of periodontal disease management can make the teeth less mobile. | |